Credentialing Services with Infocus Solutions
Credentialing Services with Infocus Solutions
Credentialing with insurance networks is the essential step healthcare providers must take to accept patients’ insurance plans. It’s the process by which medical professionals are evaluated and approved to participate in an insurance company’s network of providers. Moreover, this evaluation includes education, training, and professional experience.
Becoming an in-network provider not only enables you to bill insurance companies directly but also offers additional advantages, including:
- Referrals: Being part of an insurance network can lead to an influx of referrals from patients covered by that network.
- Preferential Reimbursement Rates: In-network providers often enjoy higher reimbursement rates, ensuring fair service compensation.
- Increased Visibility: Insurance companies include in-network providers in their web-based directories, making it easier for patients to find and choose your services.
Why Outsource Credentialing to Infocus Solutions
The credentialing process can be time-consuming and demanding, often spanning several months. Moreover, some insurance companies may not be accepting new providers. By partnering with Infocus Solutions, you can conserve valuable time and resources. Our team of experts specializes in deciphering each payer’s unique guidelines, streamlining the credentialing process for you.
Our expert team will thoroughly check every entry, leaving no room for error or outdated information. This careful approach guarantees you have the most current and up-to-date patient data available.
Establishing a private practice comes with its share of difficulties, including the ups and downs of insurance credentialing. Infocus Solutions provides expert guidance and industry knowledge to simplify the revenue cycle setup for your new practice.
We handle the cumbersome task of applying for credentialing and securing participating provider contracts with your selected insurance companies, guaranteeing a smooth transition into practice.
Credentialing for government health programs like Medicare, Medicaid, and Tricare follows standardized procedures with stringent enrollment standards. Accurate form submission and interaction with program intermediaries are essential. Infocus Solutions possesses in-depth knowledge of these requirements and manages the daunting enrollment process on your behalf, reducing the risk of application denial.
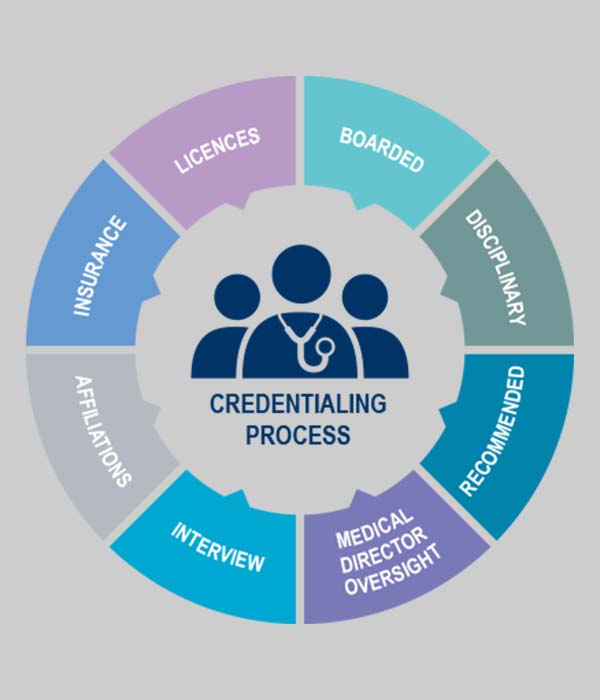
The Credentialing Process Explained
The credentialing process generally comprises two phases: credentialing and contracting.
During this phase, we assist you in submitting a participating request to your chosen health plans using their specific credentialing application process. The health insurance company carefully verifies, including a comprehensive credentialing committee review. Although this phase may span up to 90 days, our dedicated account manager provides real-time application updates, keeping you informed.
The contracting phase commences once your application receives approval and you are presented with a participation agreement. We guide you through the contract negotiations, carefully reviewing contract language, clarifying participation responsibilities, and advocating favorable reimbursement rates.
Upon agreement signing, you’ll be assigned an effective date and provider number, enabling you to bill the plan and receive in-network reimbursements.
Serving Diverse Medical Specialties
Infocus Solutions takes pride in extending our credentialing expertise to cover various medical specialties. Whether you’re a physician, hospital, or healthcare institution, our various services will address your needs. We recognize that each specialty presents distinct requirements, and our approach promises that your credentialing process aligns easily with these demands.
Infocus Solutions Makes Credentialing Simple
Trust Infocus Solutions your credentialing needs to Infocus Solutions means you’re choosing a partner dedicated to simplifying the path to becoming an in-network provider. As you focus on delivering exceptional patient care, we handle the hassles of credentialing. Contact us today to explore our services and discover how we can help!
